STATE GOVERNMENT
Bill would require insurance to cover fertility services
21 states require some fertility coverage, but not Washington
OLYMPIA (Jan. 24, 2024) — Access to fertility services and the ability to grow your family should not be reserved for the wealthy. Requiring insurance plans in Washington state to include fertility coverage would make this treatment more affordable for all.
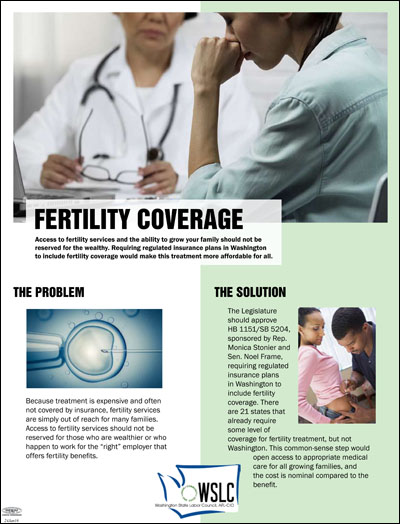 The Washington State Labor Council, AFL-CIO joins healthcare advocates in supporting passage of HB 1151, sponsored by Rep. Monica Stonier (D-Vancouver), which would require regulated insurance plans in the state to include fertility coverage. SB 5204, the Senate version, is sponsored by Sen. Noel Frame (D-Seattle).
The Washington State Labor Council, AFL-CIO joins healthcare advocates in supporting passage of HB 1151, sponsored by Rep. Monica Stonier (D-Vancouver), which would require regulated insurance plans in the state to include fertility coverage. SB 5204, the Senate version, is sponsored by Sen. Noel Frame (D-Seattle).
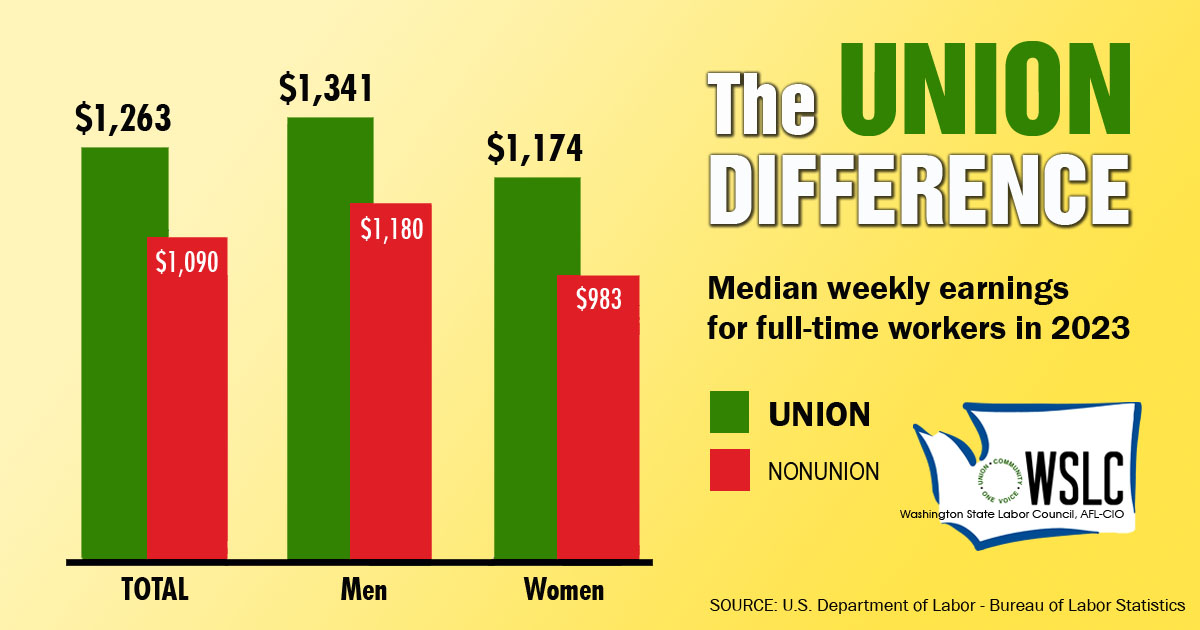
Because treatment is expensive and often not covered by insurance, fertility services are simply out of reach for many families. Access to these services should not be reserved for those who are wealthier or who happen to work for the “right” employer that offers fertility benefits.
There are 21 states that already require some level of coverage for fertility treatment, but not Washington. This common-sense step would open access to appropriate medical care for all growing families, and the cost is nominal compared to the benefit.
Last year, the House passed HB 1151 with bipartisan support, 65-30, but the bill didn’t get a vote in the Senate.
HB 1151/SB 5204 requiring regulated insurance plans in Washington to include fertility coverage is among the priority legislation in the Washington State Labor Council’s 2024 Legislative Agenda.
Here are some excerpts from the WSLC’s fact-sheet on the issue:
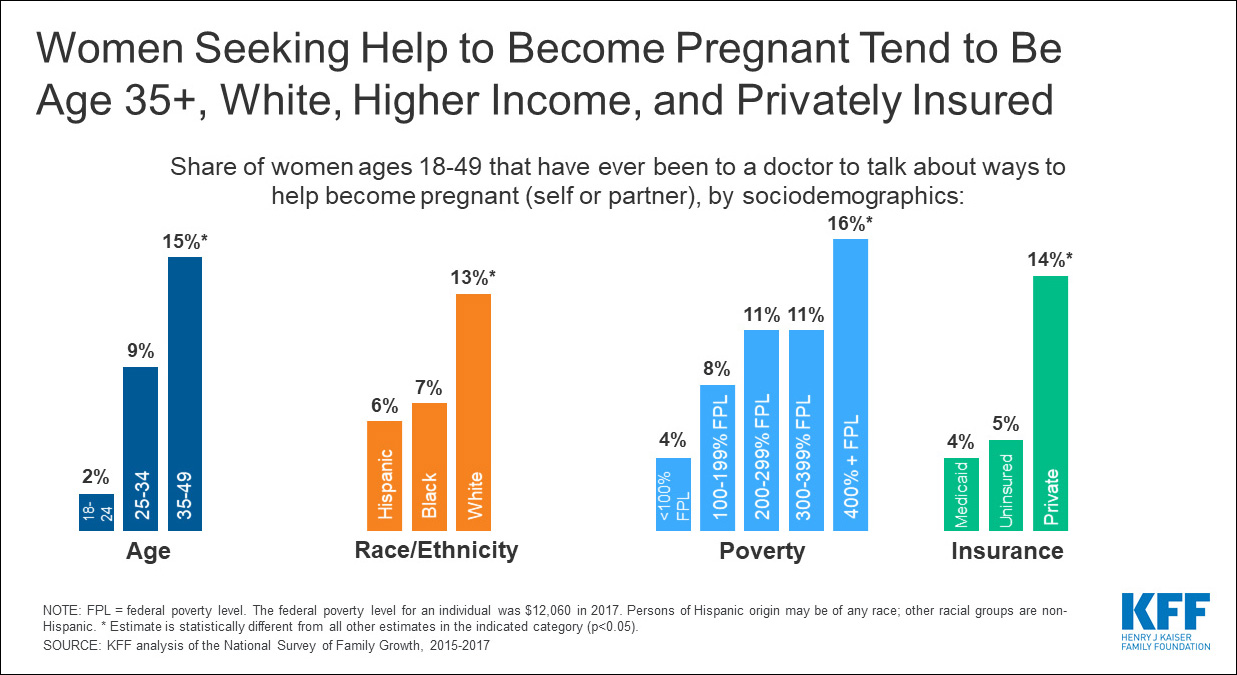
 ● The dream of building a family, of being there for a child’s first word or when they take their first steps is something many people hold dear. But with approximately 19% of women of childbearing age experiencing infertility, to say nothing of same-sex couples and single women, a biological child is not possible for many without costly fertility services.
● The dream of building a family, of being there for a child’s first word or when they take their first steps is something many people hold dear. But with approximately 19% of women of childbearing age experiencing infertility, to say nothing of same-sex couples and single women, a biological child is not possible for many without costly fertility services.
● The limited private health insurance coverage and high out-of-pocket costs for fertility services are simply out of reach for many families. Fertility services may include infertility treatment, IVF treatment, and fertility preservation, which can run more than $24,000 per treatment. A 2022 study from Duke University concluded that the cost of IVF treatment remains the greatest barrier to infertility care in the U.S., noting that the cost of each successful birth can be $60,000 or more.
● Requiring regulated insurance plans in Washington to include fertility coverage would make this treatment more affordable for parents. Twenty-one states already require some coverage for infertility treatment as of 2023, including Colorado, Illinois, Maryland, California, and Montana. A 2023 fertility treatment benefit and implementation cost analysis prepared for HCA and OIC showed increased costs averaging $3.18 per member per month across Medicaid, PEBB, SEBB, and private insurance plans.
● This is a common-sense step to expand access to appropriate medical care for all families, not just those who are wealthier or happen to work for the “right” employer that offers fertility benefits.
● Access to fertility services should not be reserved for the wealthy, and working people should be able to grow their families. For many, this means timely, affordable access to fertility care.